Important COVID-19 Information
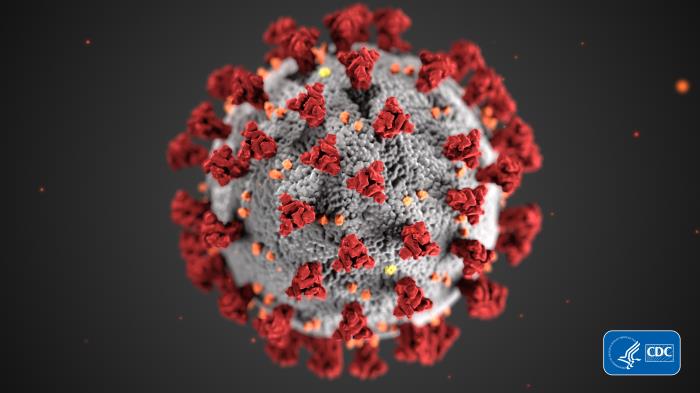
This illustration, created at the Centers for Disease Control and Prevention (CDC), reveals ultrastructural morphology exhibited by coronaviruses. Note the spikes that adorn the outer surface of the virus, which impart the look of a corona surrounding the virion, when viewed electron microscopically. A novel coronavirus, named Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2), was identified as the cause of an outbreak of respiratory illness first detected in Wuhan, China in 2019. The illness caused by this virus has been named coronavirus disease 2019 (COVID-19).
SIH’s team of infectious disease and infection prevention specialists and emergency preparedness personnel continue to collaborate with local, state and federal officials regarding COVID-19 (novel coronavirus) prevention and response. While COVID-19 is new, preparing for responses to potential epidemics and pandemics (e.g., H1N1, Swine Flu, MERS, SARS, Ebola) isn’t. In Southern Illinois, a dedicated, multidisciplinary group of professionals and community partners are in regular communication on how to provide safe, effective care for our regional community.
Within SIH, we’re providing updated, appropriate training, resources and support to our inpatient and outpatient facilities to manage suspected and/or confirmed cases of COVID-19. Proactive plans are in place should we experience a surge of patients in emergency departments at SIH Memorial Hospital of Carbondale, SIH Herrin Hospital and SIH St. Joseph Memorial Hospital in Murphysboro.
This proactive planning includes (not limited to):
- Working with the Centers for Disease Control (CDC), the Illinois Department of Public Health (IDPH) and local public health departments on the most up-to-date screening, testing and treatment recommendations
- Phone screening for patients to assess their risk and need for testing
- Signage at hospital and outpatient clinic entrances and registration desks to potential at-risk patients
- Necessary and required isolation and infection prevention protocols for patients and staff protection
- Ongoing communication with regional county health departments and regional healthcare providers
- Securing and replenishing our supply of personal protective equipment
While much remains unknown about COVID-19, a clearer picture is emerging. We’re refining our response based on new information. Our hospitals and health centers are ready: we know how to isolate patients accordingly and what services and equipment are required. When necessary, we’ll contact local and state Departments of Public Health to coordinate testing and appropriate care.
- Have a COVID-19 question? Call the Illinois Department of Public Health’s COVID-19 Hotline at 800.889.3931 or email DPH.SICK@ILLINOIS.GOV. Both resources are available 24/7.
Screening and Testing
- From what we currently know, most people who become infected with COVID-19 won’t become seriously ill and will therefore not need hospitalization. However, those with serious illness may need hospital care, including respiratory support. Symptoms reported among COVID-19 patients have included mild to severe respiratory illness with fever, cough, and difficulty breathing.
- As part of the screening process for COVID-19, healthcare providers ask patients with fever and respiratory symptoms about their travel history.
- In February, Illinois became the first state to provide COVID-19 testing in-state, allowing IDPH to produce results within 24 hours.
- The state is working with university communities to perform COVID-19 testing on 15 samples per week of patients that have had flu testing. This will help identify COVID-19 in the community early and enact control measures sooner rather than later. SIH will work with the state to provide these random samples.
Suspect Exposure to Infection of COVID-19?
Please follow the steps below to help prevent spread in your home and community:
- Call ahead before visiting your primary care physician (family doctor). If you have an appointment, please call your doctor’s office to let them know you may have or have COVID-19. Wear a facemask when around other people (e.g., sharing a room or vehicle) or pets before you enter your healthcare provider’s office.
- Monitor your symptoms. Seek prompt medical attention if your illness is worsening (e.g., difficulty breathing).
- If you have a medical emergency and need to call 9-1-1, notify the dispatch personnel that you have, or are being evaluated, for COVID-19. If possible, put on a facemask before emergency medical services arrive.
- Stay home except to receive medical care. People who are mildly ill with COVID-19 are able to isolate at home during their illness. Don’t go to work, school or public areas. Avoid using public transportation, ride-sharing or taxis.
- Separate yourself from other people and animals in your home.
- Clean all “high-touch” surfaces every day. This includes counters, tabletops, doorknobs, bathroom fixtures, phones, keyboards, tablets, remote controls and bedside tables.
- Follow CDC's recommendations for using a facemask.
- CDC does not recommend that people who are well wear a facemask to protect themselves from respiratory diseases, including COVID-19.
- Facemasks should be used by people who show symptoms of COVID-19 to help prevent the spread of the disease to others. The use of facemasks is also crucial for health workers and people who are taking care of someone in close settings (at home or in a health care facility).
- Wash your hands often and avoid touching your eyes, nose and mouth.
COVID-19 Resources
COVID-19 is spread from person-to-person by respiratory droplets, which occurs when someone who is sick coughs or sneezes. Symptoms for COVID-19 usually appear two to 14 days after initial exposure to the disease.
More details are what you need to know is available on the CDC’s website